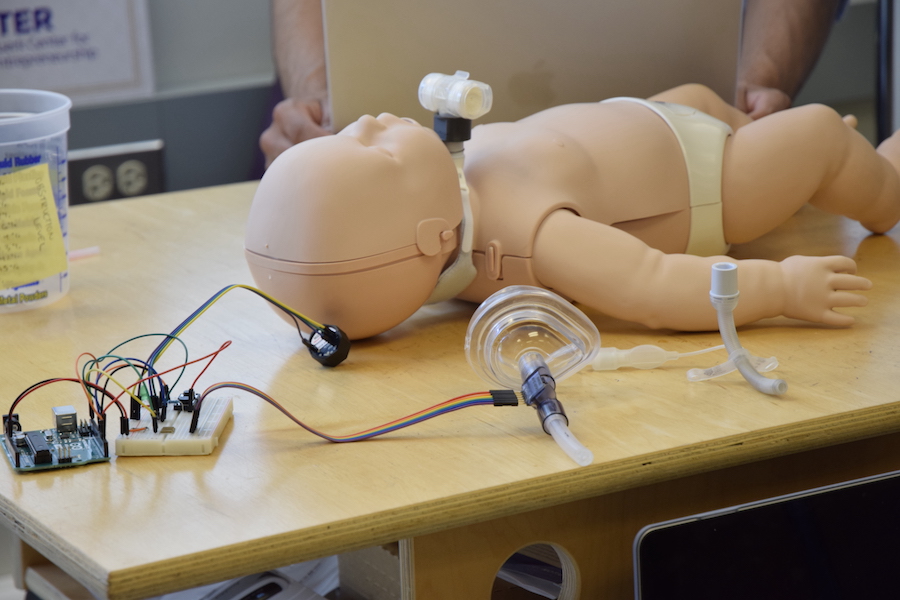
Students demonstrate how SmarTrach, a device that monitors a tracheostomy tube, works on an infant mannequin. Photo by Eli Patten.
Faculty adviser: Soyoung Kang, Clary Family Early Career Development Professor in Engineering Innovation in Health
Students: Hans Erickson, Dylan Heino, Vamsi Jonnalagadda, Clara Tamura
A child who needs help breathing might undergo a tracheostomy, a procedure that creates a small hole in the front of the neck and the windpipe. A small tube is placed into the opening and connects to a manual airbag or breathing machine. This enables the child to breathe through the tube, which they may need from months to years.
When the child returns home, a nurse or caretaker stays with them in case mucus needs to be removed from the tracheostomy tube so it doesn’t prevent them from breathing.
However, there isn’t currently an efficient way to identify when the tube is blocked. SmarTrach, an ME capstone project and Engineering Innovation in Health (EIH) collaboration, is developing a device that wirelessly monitors a tracheostomy tube and can detect blockage. An alarm sounds when air obstruction reaches intermediate or emergency levels.
The team began their preliminary work in fall 2022. “We did a deep-dive into clinical research to understand the problem and how it affects patients, parents, clinicians and hospitals,” says team member Dylan Heino.
After talking with clinicians, the team decided that measuring airflow using a hot-wire airflow sensor – instead of acoustics or vibration – was the most direct way of identifying tube blockage. They attached the sensor externally to the tracheostomy tube instead of modifying the tube’s design, which could potentially add obstruction and would need additional FDA approvals.
They tested the sensor in tubes with artificial levels of obstruction while someone breathed into a connected CPR mask. Using straws containing different materials – such as toothpaste, pipe cleaners and hot glue – they measured how well the device detected different levels of blockage.
To collect data about how the obstruction changed airflow, the team developed a specialized algorithm. “We didn’t have coding experience, so we had to learn how to write code to implement it into our device,” says team member Clara Tamura. “It involved lots of trial and error.”
They worked with one of their mentors, Andrew Davidson, associate teaching professor in Human Centered Design & Engineering, to implement their code and include a button, triggers and an alarm into the tiny device.
In addition to creating the device, the students learned about the process of commercializing medical devices. They became familiar with FDA regulations, created a five-year financial plan and estimated manufacturing costs. At the 2023 Hollomon Health Challenge, the students were recognized for their work with the Best Idea Prize for patient safety.
Originally published August 17, 2023